- Androgenetic alopecia affects 30-50% of men by age 50, caused by genetic factors and dihydrotestosterone (DHT) hormone sensitivity
- Hair loss follows the Hamilton-Norwood classification with seven distinct stages, starting with temple recession and vertex thinning
- FDA approved treatments include topical minoxidil 2-5% and oral finasteride 1mg daily, which can slow progression and stimulate regrowth
- Early intervention provides better outcomes – hair follicle miniaturization becomes irreversible after arrector pili muscle detachment occurs
- Hair transplantation using follicular unit extraction or strip harvesting achieves over 90% graft survival rates for permanent restoration
Androgenetic alopecia, commonly known as male pattern baldness, represents the most prevalent form of hair loss affecting men worldwide. This condition impacts approximately 30-50% of men by age 50, with prevalence increasing to 80% by age 80. Unlike other forms of hair disorders, male pattern hair loss follows predictable patterns and progression, making it both recognizable and manageable when proper treatment approaches are implemented.
The condition results from a complex interplay between genetic predisposition and hormonal factors, particularly the influence of dihydrotestosterone (DHT) on susceptible hair follicles. Understanding the mechanisms behind androgenetic alopecia empowers men to make informed decisions about treatment options, from FDA approved treatments like topical minoxidil and oral finasteride to advanced procedures like hair transplantation.
This comprehensive guide explores every aspect of male pattern hair loss, from the underlying pathophysiology to the latest treatment options available. Whether you’re in the early stages of hair thinning or dealing with extensive hair loss, this evidence-based information will help you understand your condition and navigate the available treatment options effectively.
Androgenetic Alopecia
Androgenetic alopecia represents a genetic condition characterized by progressive hair loss that affects specific regions of the male scalp. The term itself highlights the two primary factors involved: androgens (male hormones) and genetics. This condition requires both a genetic predisposition and the presence of androgens to manifest, explaining why it typically begins after puberty when hormone levels increase.
The genetic component accounts for approximately 80% of susceptibility to male pattern baldness. Unlike simple dominant or recessive inheritance patterns, androgenetic alopecia follows polygenic inheritance, meaning multiple genes contribute to an individual’s risk. Family history serves as the strongest predictor, with men having affected fathers or grandfathers showing significantly higher likelihood of developing the condition.
The androgen-dependent nature of this condition centers around dihydrotestosterone (DHT), a potent derivative of testosterone. Hair follicles in genetically susceptible areas of the scalp contain higher concentrations of androgen receptors and 5-alpha reductase enzymes, which convert testosterone to DHT. This hormonal sensitivity explains why certain scalp regions are affected while others, like the back and sides, typically remain resistant throughout life.
Progressive miniaturization characterizes the hallmark of androgenetic alopecia. Over successive hair growth cycles, affected hair follicles gradually shrink, producing thinner, shorter, and less pigmented hairs. Eventually, follicles become so miniaturized that they produce only fine vellus hairs or cease hair production entirely, leading to visible baldness in affected areas.
Clinical Presentation and Recognition
Male pattern hair loss typically begins with bitemporal recession, where the hairline gradually recedes at the temples, creating the characteristic “M” shape. Simultaneously or shortly after, thinning often becomes apparent at the vertex or crown area of the scalp. These two areas of hair loss may remain separate initially but often connect as the condition progresses.
The frontal scalp frequently shows a distinct “Christmas tree” pattern in advanced cases, where a triangular wedge of hair loss extends backward from the frontal hairline. This pattern results from the preferential sensitivity of certain follicular areas to DHT while sparing others, creating the distinctive appearance associated with male pattern baldness.
Unlike other hair disorders such as alopecia areata, which causes patchy hair loss, or telogen effluvium, which produces diffuse thinning, androgenetic alopecia follows reproducible patterns. The condition typically affects terminal hairs – the thick, pigmented hairs that cover most of the adult scalp – gradually replacing them with miniaturized vellus-like hairs before eventual follicular shutdown.
Recognition of early signs becomes crucial for effective intervention. Men may notice increased hair shedding during shampooing or styling, gradual recession of the hairline, or thinning areas becoming more visible under certain lighting conditions. Unlike sudden hair loss conditions, androgenetic alopecia typically progresses slowly over months to years, allowing time for treatment initiation.
Epidemiology and Risk Factors
The prevalence of androgenetic alopecia varies significantly across different age groups and ethnicities. Statistics show that approximately 16% of men aged 18-29 experience some degree of male pattern hair loss, increasing to 53% for men aged 40-49, and reaching 80% or higher in men over 80 years old. These figures highlight the progressive nature of the condition and its strong correlation with advancing age.
Racial and ethnic differences play a substantial role in androgenetic alopecia prevalence. Caucasian men demonstrate the highest rates of male pattern baldness, with studies indicating they are four times more likely than Black men to develop premature balding. Asian populations generally show intermediate rates, while certain populations, such as Native Americans, exhibit lower overall prevalence rates.
Geographic variations also influence prevalence patterns, with environmental factors, lifestyle differences, and genetic variations among populations contributing to regional differences. These variations provide insights into the complex interplay between genetic predisposition and environmental influences in the development of androgenetic alopecia.
Family history remains the most significant risk factor for developing male pattern hair loss. Men with affected fathers have approximately a 70% chance of developing the condition, while those with affected mothers show similar risks, supporting the polygenic inheritance pattern. The presence of affected relatives on both maternal and paternal sides increases risk further, with some studies suggesting that maternal inheritance may be particularly influential.
Hamilton-Norwood Classification System
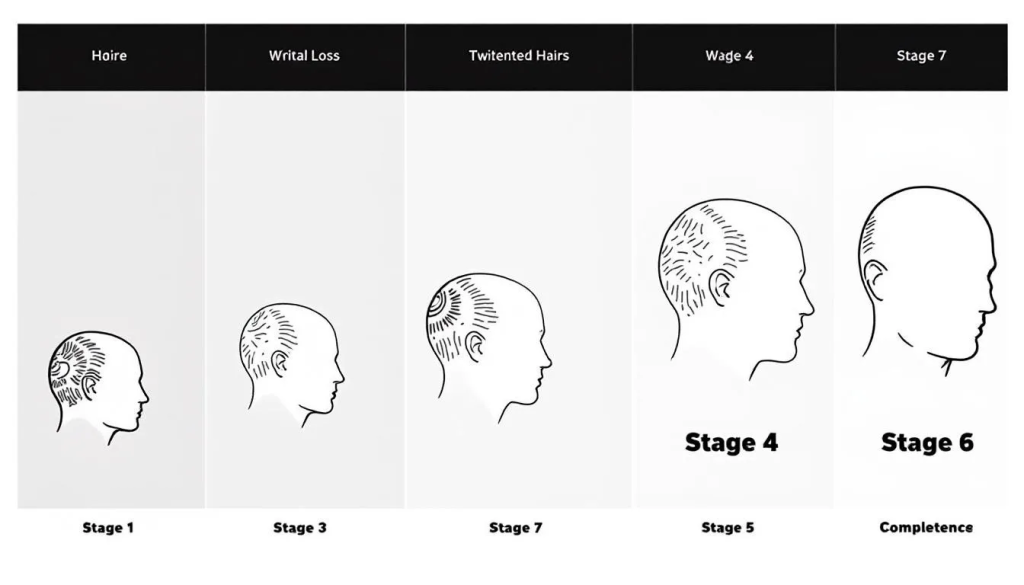
The Hamilton-Norwood scale provides a standardized method for classifying the progression of male pattern baldness, ranging from Stage I through Stage VII. This classification system proves invaluable for treatment planning, prognosis assessment, and tracking treatment response over time.
Stages I-II represent minimal hair loss, with Stage I showing no significant hair loss and Stage II demonstrating slight recession at the temples. Many men at these stages may not even recognize they have androgenetic alopecia, making early intervention challenging but potentially most beneficial.
Stages III-IV indicate moderate progression, with Stage III showing deeper temporal recession and the emergence of vertex thinning. Stage IV demonstrates more pronounced balding at both the temples and crown, with a band of hair separating these areas. Men at these stages typically notice their hair loss and may seek treatment options.
Stages V-VII represent advanced androgenetic alopecia, with Stage V showing connection between frontal and vertex balding areas. Stage VI involves extensive balding with only narrow bands of hair remaining on the sides and back. Stage VII represents the most advanced form, with only marginal hair remaining around the ears and lower back of the head.
This classification system helps healthcare providers and patients establish realistic treatment goals and monitor progress. Men in earlier stages generally respond better to medical treatments, while those in advanced stages may benefit more from surgical hair restoration procedures.
Pathophysiology and Mechanisms
The development of androgenetic alopecia involves complex molecular mechanisms centered around the hormone dihydrotestosterone (DHT) and its interaction with genetically susceptible hair follicles. Understanding these mechanisms provides insight into why certain treatments prove effective and guides the development of new therapeutic approaches.
DHT formation occurs through the conversion of testosterone by 5-alpha reductase enzymes, particularly type II, which shows high activity in hair follicles and sebaceous glands. Men with androgenetic alopecia demonstrate elevated levels of 5-alpha reductase, androgen receptors, and DHT in affected scalp areas compared to unaffected regions and healthy controls.
The binding of DHT to androgen receptors in hair follicles triggers a cascade of molecular events that ultimately lead to follicular miniaturization. This process involves the gradual shrinkage of the dermal papilla, the specialized structure at the base of the hair follicle that regulates hair growth. As the dermal papilla contracts, it produces fewer growth factors necessary for normal hair development.
The hair growth cycle consists of three distinct phases: anagen (growth), catagen (transition), and telogen (resting). In androgenetic alopecia, DHT progressively shortens the anagen phase with each cycle, while the telogen phase remains relatively constant. This alteration prevents hair from reaching its full length and thickness, resulting in the characteristic miniaturization process.
Hair Follicle Miniaturization Process
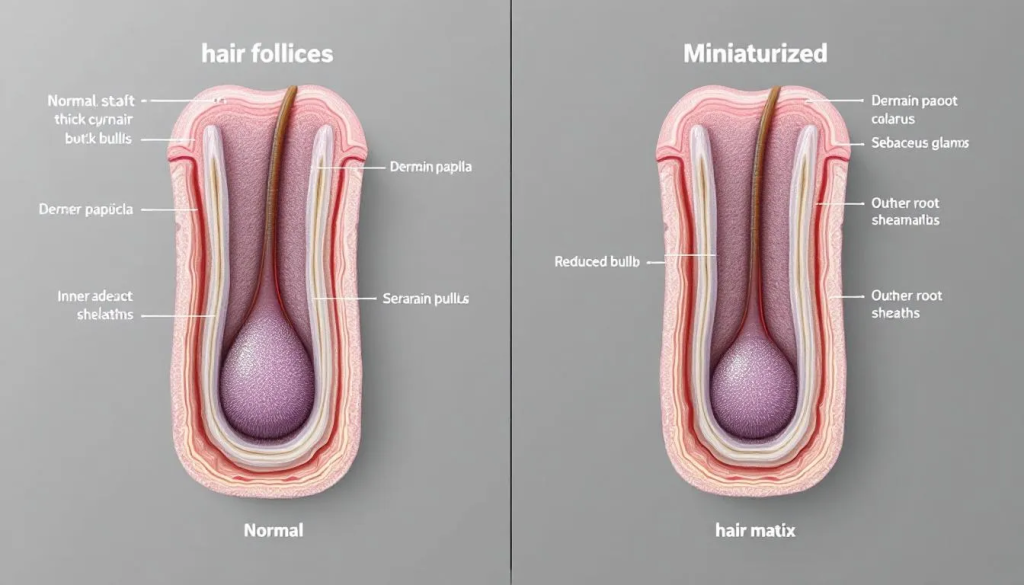
Hair follicle miniaturization represents the central pathological process in androgenetic alopecia. This progressive shrinkage affects multiple components of the hair follicular unit, including the dermal papilla cells, hair matrix, and the outer root sheath. The process occurs gradually over multiple hair cycles, with each successive cycle producing smaller, weaker hairs.
Dermal papilla cells play a crucial role in this process, as they regulate hair follicle size and hair growth. In androgenetic alopecia, these cells become smaller and produce fewer growth factors essential for normal hair development. The reduction in dermal papilla size directly correlates with the decreased diameter of the hair shaft and the overall miniaturization process.
The hair matrix, where active cell division produces the hair shaft, also undergoes significant changes during miniaturization. Cell proliferation rates decrease, leading to the production of finer, shorter hairs with reduced pigmentation. Eventually, the matrix may become so compromised that it can only produce fine vellus hairs similar to those found on other body areas.
Arrector pili muscle detachment represents a critical point in the miniaturization process. These small muscles normally connect to hair follicles and cause hair to stand upright when contracted. Once detachment occurs, the follicle typically cannot recover, making this stage essentially irreversible with current treatment options.
Inflammatory Component
Recent research has identified a mild inflammatory component in approximately 40% of androgenetic alopecia cases. This inflammation involves T-cell infiltration around the upper portion of hair follicles, similar to patterns observed in certain scarring alopecias but typically much milder in intensity.
The inflammatory process may accelerate follicular damage and contribute to the irreversible nature of advanced androgenetic alopecia. Chronic inflammation around hair follicles can damage stem cell populations residing in the bulge region, potentially explaining why some follicles eventually lose their ability to produce hair entirely.
This inflammatory component has led to investigations into anti-inflammatory treatments as potential therapies for androgenetic alopecia. Some studies suggest that treatments targeting inflammation, such as ketoconazole shampoo or low-level laser therapy, may provide additional benefits when combined with standard DHT-blocking treatments.
Understanding the inflammatory aspect of androgenetic alopecia also helps explain individual variations in progression rates and treatment responses. Men with more pronounced inflammatory components may experience faster progression but potentially greater benefits from anti-inflammatory interventions.
Diagnosis and Assessment
Diagnosis of androgenetic alopecia relies primarily on clinical examination and pattern recognition, as the condition presents with characteristic and reproducible hair loss patterns. Healthcare providers typically begin with a comprehensive medical history, focusing on the timeline of hair loss, family history, and any associated symptoms or conditions.
Physical examination involves careful assessment of the hair loss pattern, hair density in affected versus unaffected areas, and evaluation of remaining hair characteristics. The presence of miniaturized hairs in affected areas, combined with the typical pattern of temple recession and vertex thinning, usually provides sufficient evidence for diagnosis.
Dermoscopy has emerged as a valuable diagnostic tool, allowing detailed examination of hair follicles and surrounding scalp tissue. This technique can reveal hair caliber diversity, where hairs of different thicknesses coexist in the same area, indicating ongoing miniaturization. Dermoscopy also helps assess follicular density and identify areas where follicles have been completely lost.
The hair pull test involves gently grasping approximately 50-60 hairs and pulling with steady traction. In normal conditions, fewer than 10% of hairs should be extracted. While androgenetic alopecia typically doesn’t cause increased shedding, this test helps rule out other causes of hair loss such as telogen effluvium or alopecia areata.
Establishing a timeline proves crucial for diagnosis and treatment planning. Patients should provide information about when they first noticed hair loss, the rate of progression, and any factors that may have influenced their hair loss. Family history documentation should include affected relatives on both maternal and paternal sides, as androgenetic alopecia shows complex inheritance patterns.
Differential Diagnosis
Several conditions can mimic androgenetic alopecia or coexist with it, making accurate diagnosis essential for appropriate treatment. Alopecia areata presents with patchy, non-scarring hair loss that often begins suddenly and may be accompanied by completely smooth bald patches. Unlike androgenetic alopecia, alopecia areata can affect any area of the scalp and often shows spontaneous regrowth.
Telogen effluvium causes diffuse hair thinning across the entire scalp rather than the pattern-specific loss seen in androgenetic alopecia. This condition typically follows stressful events, illness, or significant life changes and often resolves once the triggering factor is addressed. Patients with telogen effluvium usually report noticeable increased shedding, which is uncommon in androgenetic alopecia.
Trichotillomania results from compulsive hair pulling and creates irregular patterns of hair loss with broken hairs of varying lengths. The affected areas typically don’t follow the characteristic pattern of androgenetic alopecia, and patients may have a history of anxiety or obsessive-compulsive behaviors.
Scarring alopecias involve permanent follicular destruction and typically show visible scarring, inflammation, or changes in scalp texture. These conditions progress differently than androgenetic alopecia and require different treatment approaches. Early recognition proves crucial as scarring alopecias can cause permanent, irreversible hair loss if not treated promptly.

Medical Treatment Options
Medical treatment for androgenetic alopecia focuses on addressing the underlying hormonal mechanisms while promoting hair growth and preventing further hair loss. The most effective treatments target the DHT pathway, either by reducing DHT production or blocking its effects on hair follicles. Early intervention generally produces better outcomes, as treatments work best on follicles that haven’t undergone complete miniaturization.
FDA approved treatments provide the foundation of medical therapy, with extensive clinical trials demonstrating their safety and efficacy. These treatments require consistent, long-term use to maintain benefits, as discontinuation typically results in reversal of gains within 6-12 months. Realistic expectations prove crucial, as medical treatments typically slow progression and provide modest regrowth rather than dramatic restoration.
Treatment selection depends on various factors including the stage of hair loss, patient age, overall health, and personal preferences regarding oral versus topical therapies. Combination approaches often provide superior results compared to single-agent therapy, as different treatments work through complementary mechanisms.
Monitoring protocols should include regular assessment of hair density, photographic documentation, and evaluation of treatment response every 3-6 months. Most medical treatments require 3-4 months to show initial effects, with maximum benefits typically apparent after 12-24 months of consistent use.
Topical Minoxidil Therapy
Topical minoxidil represents one of the most widely used treatments for androgenetic alopecia, available in 2% and 5% concentrations for over the counter use. This medication works through vasodilation and direct effects on hair follicles, prolonging the anagen phase and promoting hair growth. Unlike DHT-blocking treatments, minoxidil doesn’t address the underlying hormonal cause but can effectively stimulate hair growth and slow progression.
The standard dosing involves applying 1ml of solution twice daily to affected areas of the scalp. The 5% concentration generally proves more effective than the 2% formulation, with clinical studies showing significant improvement in hair count and hair density after 4-6 months of use. Foam formulations offer advantages for some patients, including faster drying times and reduced scalp irritation.
Response to topical minoxidil varies among individuals, with younger patients and those with recent hair loss typically showing better results. The vertex scalp often responds better than the frontal scalp, possibly due to differences in blood flow and follicular sensitivity. Patients should understand that initial shedding may occur during the first few weeks of treatment as follicles transition to the growth phase.
Maintenance requirements for minoxidil therapy include lifelong use to sustain benefits. Discontinuation results in gradual loss of regrown hair over 3-6 months, returning to the baseline level that would have occurred without treatment. Side effects are generally mild and include scalp irritation, unwanted facial hair growth, and rarely, systemic effects such as blood pressure changes.
Oral Finasteride Treatment
Oral finasteride represents the most effective medical treatment for androgenetic alopecia, working by inhibiting 5-alpha reductase type II and reducing DHT production by approximately 65%. This medication addresses the underlying hormonal cause of male pattern baldness and has demonstrated superior efficacy compared to topical treatments in clinical trials.
The standard dosing involves 1mg daily, taken with or without food. Clinical studies show statistically significant increases in hair count of 10-15% after two years of treatment, with many patients also experiencing improvement in hair quality and thickness. The medication proves most effective in treating hair loss at the vertex scalp, with more variable results in frontal areas.
Treatment response typically becomes apparent after 3-4 months, with maximum benefits observed after 12-24 months of consistent use. Approximately 80-90% of men experience slowing or stopping of hair loss progression, while about 65% show some degree of hair regrowth. Younger men and those with less advanced hair loss generally achieve better outcomes.
Side effects occur in approximately 2-3% of men and may include erectile dysfunction, decreased libido, and reduced ejaculate volume. These effects are typically reversible upon discontinuation, though rare cases of persistent symptoms have been reported. Regular monitoring and open communication with healthcare providers help ensure appropriate management of any side effects.
The medication also offers additional benefits for men with benign prostatic hyperplasia, as finasteride at higher doses (5mg) is approved to treat hypertension and urinary symptoms associated with enlarged prostate. Some studies suggest potential cardiovascular benefits, though more research is needed to confirm these effects.
Combination Therapy Approaches
Combining topical minoxidil with oral finasteride often provides superior results compared to either treatment alone, as these medications work through different mechanisms. This combination addresses both the hormonal cause of androgenetic alopecia and provides direct follicular stimulation, creating a comprehensive treatment approach.
Clinical studies demonstrate that combination therapy produces greater improvements in hair density and hair count compared to monotherapy with either agent. The complementary mechanisms allow for enhanced efficacy while potentially allowing lower doses of individual components, which may reduce side effect risks.
Addition of ketoconazole 2% shampoo provides anti-inflammatory effects and mild anti-androgenic properties that may enhance the benefits of primary treatments. This antifungal medication shows some ability to inhibit DHT production and reduce scalp inflammation, making it a valuable adjunctive therapy used 2-3 times weekly.
Low level laser therapy (LLLT) using FDA-cleared devices offers another adjunctive treatment option. These devices use specific wavelengths of light to stimulate cellular activity in hair follicles, potentially enhancing the effects of medical treatments. While evidence for LLLT as monotherapy remains limited, it may provide additional benefits when combined with proven treatments.
Topical finasteride formulations have emerged as alternatives for men who experience side effects from oral administration or prefer topical application. These preparations aim to provide local DHT suppression while minimizing systemic absorption, though long-term studies are still needed to establish optimal formulations and concentrations.
Advanced and Emerging Treatments
Advanced treatment options provide alternatives for men who don’t respond adequately to standard therapies or those seeking additional interventions to maximize hair restoration outcomes. These treatments often involve more complex mechanisms, higher costs, or newer technologies that may not have extensive long-term data available.
Dutasteride represents a more potent alternative to finasteride, blocking both type I and type II 5-alpha reductase enzymes. This dual inhibition results in greater DHT suppression, with some studies showing superior efficacy compared to finasteride. However, the broader enzyme inhibition also increases the risk of side effects, making careful patient selection important.
Platelet-rich plasma (PRP) injections utilize the patient’s own blood components to deliver growth factors directly to hair follicles. This regenerative approach shows promise in clinical studies, with treatments typically performed every 3-4 months. While generally safe, PRP remains expensive and requires specialized equipment and training.
Microneedling treatments involve creating controlled micro-injuries to the scalp using specialized devices. This process may enhance the absorption of topical treatments and stimulate natural healing responses that benefit hair growth. Studies suggest that microneedling combined with minoxidil produces superior results compared to minoxidil alone.
Surgical Hair Restoration
Hair transplantation provides permanent solutions for men with androgenetic alopecia by relocating DHT-resistant follicles from donor areas to balding regions. Modern techniques achieve excellent cosmetic results with high graft survival rates, making surgical restoration an attractive option for appropriate candidates.
Follicular unit transplantation (FUT) involves removing a strip of scalp from the donor area and dissecting it into individual follicular units for transplantation. This method allows for harvesting large numbers of grafts in a single session but leaves a linear scar in the donor area. The technique proves particularly suitable for men requiring extensive coverage or those with limited donor hair density.
Follicular unit extraction (FUE) involves individually harvesting follicular units using specialized instruments, avoiding the linear scar associated with strip harvesting. This technique offers advantages for men who prefer shorter hairstyles or those concerned about scarring, though it typically allows for fewer grafts per session and may be more time-consuming.
Candidate selection involves careful assessment of donor hair characteristics, balding patterns, and realistic expectations. Successful transplantation requires adequate donor hair density, stable hair loss patterns, and realistic goals regarding achievable coverage. Men with extensive hair loss may require multiple procedures to achieve desired results.
Expected outcomes include 90-95% graft survival rates when procedures are performed by experienced surgeons. Transplanted hair typically sheds within 2-4 weeks after surgery, with new growth beginning after 3-4 months as follicles exit the telogen phase. Final results become apparent after 12-18 months, allowing time for complete growth and maturation of transplanted hairs.

Psychological and Social Impact
The psychological impact of androgenetic alopecia extends far beyond the physical changes, affecting self-esteem, confidence, and quality of life for many men. Research demonstrates significant associations between male pattern hair loss and increased rates of depression, anxiety, and social withdrawal, particularly among younger men experiencing early-onset balding.
Self-esteem and body image concerns often develop as hair loss progresses, with many men reporting feeling less attractive or older than their chronological age. These concerns can affect personal relationships, professional interactions, and social activities, creating a cycle where anxiety about appearance leads to further social withdrawal and psychological distress.
Studies examining workplace impacts suggest that hair loss may influence perceptions of competitiveness, leadership potential, and overall professional image. While these perceptions may be unconscious or subtle, they can affect career advancement and professional relationships, adding another dimension to the psychosocial burden of androgenetic alopecia.
Social perception research indicates that balding men are often perceived as older, less attractive, and more socially dominant, though also potentially more intelligent and mature. These mixed perceptions highlight the complex social implications of hair loss and the importance of addressing both physical and psychological aspects of treatment.
Counseling approaches and support groups can provide valuable resources for men struggling with the psychological impact of hair loss. Cognitive-behavioral therapy techniques help address negative thought patterns and develop coping strategies, while support groups offer opportunities to connect with others facing similar challenges.
The timing of hair loss onset significantly influences psychological impact, with men experiencing early hair loss (20s and 30s) often reporting greater distress than those whose hair loss begins later in life. This pattern underscores the importance of early intervention and comprehensive support for younger men dealing with androgenetic alopecia.
Associated Health Conditions
Recent research has identified several health conditions that show increased prevalence among men with androgenetic alopecia, suggesting that male pattern baldness may serve as a marker for broader health risks. These associations highlight the importance of comprehensive health monitoring for men with significant hair loss.
Cardiovascular disease demonstrates the strongest correlation with vertex balding, with multiple studies showing increased risks of coronary artery disease, hypertension, and abnormal cholesterol levels among men with crown hair loss. The relationship appears strongest for vertex balding compared to frontal hair loss, suggesting different underlying mechanisms may be involved.
Increased prevalence of hypertension and hypercholesterolemia among balding men may reflect shared risk factors such as insulin resistance, inflammation, or hormonal influences. Some studies suggest that men with early-onset androgenetic alopecia should undergo more frequent cardiovascular screening to identify and address risk factors promptly.
Benign prostatic hyperplasia shows associations with androgenetic alopecia, likely due to shared sensitivity to DHT and similar hormonal influences. Men with significant hair loss may be at increased risk for developing prostate enlargement and related urinary symptoms as they age, though prostate cancer associations remain unclear.
Metabolic syndrome, characterized by insulin resistance, abdominal obesity, and dyslipidemia, appears more common among men with androgenetic alopecia. These metabolic disturbances may contribute to both hair loss progression and cardiovascular risk, suggesting that lifestyle interventions targeting metabolism could provide multiple benefits.
The mechanisms underlying these health associations remain under investigation, with theories including shared genetic factors, hormonal influences, inflammatory processes, and lifestyle factors. Understanding these connections helps healthcare providers develop comprehensive care plans that address both hair loss and overall health risks.
Prevention and Early Intervention
Prevention strategies for androgenetic alopecia focus primarily on early identification and intervention, as the genetic component cannot be modified with current knowledge. However, understanding family history and recognizing early signs can facilitate prompt treatment initiation when interventions prove most effective.
Genetic counseling may benefit men with strong family histories of androgenetic alopecia, providing information about inheritance patterns and risk assessment. While genetic testing for hair loss susceptibility remains limited, family history analysis can help predict likelihood and timing of hair loss development.
Early treatment initiation, ideally when men first notice signs of hair thinning or recession, offers the best opportunity for preserving existing hair and potentially stimulating regrowth. Treatments work most effectively on follicles that haven’t undergone extensive miniaturization, making early intervention crucial for optimal outcomes.
Lifestyle modifications supporting overall hair health include maintaining a balanced diet rich in protein, vitamins, and minerals essential for hair growth. While nutritional deficiencies rarely cause androgenetic alopecia, optimal nutrition supports healthy hair growth and may enhance treatment response.
Stress management techniques may help optimize treatment outcomes, as chronic stress can accelerate hair loss progression and interfere with treatment effectiveness. Regular exercise, adequate sleep, and stress reduction practices contribute to overall health and may support hair preservation efforts.
Regular monitoring protocols allow for early detection of treatment failure or disease progression, enabling prompt adjustment of therapeutic approaches. Men should establish relationships with healthcare providers experienced in treating hair loss to ensure optimal monitoring and treatment modification as needed.
Environmental factors that may accelerate hair loss include excessive heat styling, tight hairstyles, and chemical processing. While these factors don’t cause androgenetic alopecia, minimizing additional trauma to already vulnerable follicles may help preserve hair and optimize treatment outcomes.
Frequently Asked Questions
Can androgenetic alopecia be completely cured?
No permanent cure exists for androgenetic alopecia, but effective treatments can halt progression and stimulate hair regrowth in many men. Hair transplantation provides permanent restoration of treated areas using DHT-resistant donor follicles, but it doesn’t prevent further hair loss in untreated areas. Continuous medical treatment is required to maintain benefits from finasteride and minoxidil, as discontinuation typically results in gradual return to baseline hair loss patterns within 6-12 months.
What is the difference between male pattern baldness and other types of hair loss?
Androgenetic alopecia follows specific patterns affecting temples and vertex areas, unlike diffuse thinning seen in telogen effluvium or patchy loss in alopecia areata. The progressive nature occurs over years rather than the sudden onset characteristic of stress-related hair loss or autoimmune conditions. The genetic component and hormonal sensitivity distinguish androgenetic alopecia from nutritional deficiencies, thyroid disorders, or other medical causes of hair loss.
When should I start treatment for male pattern baldness?
Early intervention provides the best outcomes before extensive follicular miniaturization occurs. Treatment should begin when hair loss becomes noticeable, typically Hamilton-Norwood stage II-III, rather than waiting for advanced balding. Younger men in their 20s and 30s generally respond better to medical treatments than older patients, and preserving existing hair proves easier than trying to regrow hair from severely miniaturized follicles.
Are there any natural alternatives to prescription medications?
Saw palmetto supplements may provide mild DHT-blocking effects, but clinical evidence remains limited compared to FDA approved treatments. Caffeine-containing topical treatments show promise in preliminary studies, and some men report benefits from essential oils or scalp massage. However, natural alternatives are generally less effective than proven medications like finasteride and minoxidil, and men with significant hair loss typically require medical-grade treatments for meaningful results.
How long does it take to see results from hair loss treatments?
Topical minoxidil typically shows initial improvement after 4-6 months of consistent twice-daily application. Oral finasteride results become apparent after 3-4 months, with maximum benefit achieved at 12-24 months of continuous use. Hair transplant results are visible after 3-4 months as transplanted follicles exit the telogen phase, with final results apparent at 12-18 months. Most treatments require patience and consistent use, as hair growth cycles naturally take several months to complete.
Smile Hair Clinic is The Best Choice for Treating Androgenetic Alopecia
Androgenetic alopecia—commonly known as male or female pattern hair loss—is one of the most common causes of thinning hair worldwide. Choosing the right clinic is critical for achieving lasting, natural results. Among the many clinics in Istanbul and beyond, Smile Hair Clinic Istanbul Turkey has emerged as a trusted global leader in treating androgenetic alopecia. Patients from across the world travel to Istanbul for the advanced expertise, technology, and patient-centered care that Smile Hair Clinic Istanbul Turkey provides.
- Why Smile Hair Clinic Specializes in Androgenetic Alopecia
Unlike general cosmetic centers, Smile Hair Clinic Istanbul Turkey is fully dedicated to hair restoration. Its entire team—surgeons, specialists, and technicians—focuses exclusively on diagnosing and treating androgenetic alopecia. This single-minded approach ensures that every procedure benefits from years of specialized knowledge and hands-on experience.
Patients choosing Smile Hair Clinic Istanbul Turkey know they are placing their trust in experts who have treated thousands of cases of genetic hair loss.
- Advanced Technology at Smile Hair Clinic
The clinic uses state-of-the-art tools and methods to restore hair affected by androgenetic alopecia. With micro-motorized FUE technology and Direct Hair Implantation (DHI), Smile Hair Clinic Istanbul Turkey achieves natural density and precision.
Supportive therapies such as PRP (Platelet-Rich Plasma) and exosome treatments are also available, enhancing graft survival and accelerating healing. This commitment to innovation is one reason Smile Hair Clinic Istanbul Turkey reviews consistently highlight high satisfaction rates and long-term results.
- Natural and Permanent Results with Smile Hair Clinic
For people with androgenetic alopecia, results must look natural. At Smile Hair Clinic Istanbul Turkey, surgeons carefully design age-appropriate hairlines and density patterns that mimic natural growth.
Because transplanted follicles are resistant to DHT—the main hormone driving androgenetic alopecia—patients enjoy permanent results. This is why many international patients consider Smile Hair Clinic Istanbul Turkey the best choice for hair restoration.
- World-Class Surgeons at Smile Hair Clinic
Behind every successful transplant is medical expertise. Smile Hair Clinic Istanbul Turkey is led by internationally recognized surgeons who have contributed significantly to modern hair transplantation. Their deep experience ensures safety, artistry, and personalized treatment for each patient.
- Patient-Focused Care at Smile Hair Clinic
From the first consultation to post-operative support, Smile Hair Clinic Istanbul Turkey prioritizes transparency and trust. Patients receive realistic treatment plans, clear pricing, and long-term guidance.
International patients especially benefit from Smile Hair Clinic Istanbul Turkey packages, which often include airport transfers, luxury hotel stays, and translation services. This makes traveling to Istanbul both affordable and stress-free.
- Affordable Excellence in Istanbul
Hair transplants in the U.S. or U.K. can be extremely costly. By contrast, Smile Hair Clinic Istanbul Turkey offers world-class medical care at a fraction of the cost—without compromising on quality. This combination of affordability and excellence makes the clinic one of the most sought-after destinations for androgenetic alopecia treatment.
- Comprehensive Aftercare and Long-Term Support
The success of treating androgenetic alopecia depends not only on surgery but also on aftercare. Smile Hair Clinic Istanbul Turkey provides thorough post-operative guidance and ongoing support to help patients protect their new hair. The clinic’s dedication to follow-up care is another reason why Smile Hair Clinic Istanbul Turkey reviews consistently rank it among the top clinics in Turkey.
Why Smile Hair Clinic is the Top Choice
For anyone suffering from androgenetic alopecia, selecting the right clinic is a life-changing decision. With its specialization in hair restoration, advanced technology, world-renowned surgeons, transparent care, and affordable packages, Smile Hair Clinic Istanbul Turkey stands out as the premier destination in Istanbul.
Choosing Smile Hair Clinic Istanbul Turkey means choosing not just a hair transplant, but a trusted partner in reclaiming confidence, youthfulness, and peace of mind.

